Prostatitis is an inflammation of the prostate that is caused by various infections. It often flows in an acute form and is accompanied by a rise in temperature up to 37-38⁰C, pain in the perineum and problems with urination.
Untreated acute prostatitis becomes chronic and in this condition is the most common. In this case, the symptoms are less pronounced (pain in the lower abdomen, when urinating, sexual disorders, general weakening of the body) or are completely absent. However, the consequences can be very serious. The inflammatory process is directly related to potency problems and is expressed in the reduction of libido, the obliteration of orgasm.
Neglected infection dramatically increases the chances of developing complications. Specifically, these are diseases such as:
- pyelonephritis;
- cystitis;
- prostate abscess;
- BPH;
- infertility.
You can avoid such consequences if you consult a doctor in time. Take care of your health now - and in return you will receive excellent health, psychological comfort and increased self-esteem, quality of sexual relations.
Causes of prostatitis
This question is relevant not only because many men face this problem, but also because most of them cannot understand where this disease came from.
Causes of prostatitis in men:
- Sexually transmitted infections.
- Inflammatory diseases of the urethra caused by conditionally pathogenic flora.
- Sexual arrhythmia is an irregular, unbalanced sex life.
- Physical inactivity is a sedentary lifestyle.
- Urolithiasis disease.
- The presence of foci of chronic infection in the body (chronic tonsillitis, pharyngitis, sinusitis, proctitis and paraproctitis, etc. ).
- Abuse of alcohol and spicy food.
- Prison.
- Hypothermia.
- Pathology of the lumbosacral spine and spinal cord - due to violation of innervation and trophism of the prostate.
Why does prostatitis occur when an STI is contracted? Agents of genital infections, especially such as gonococcus, trichomonas, chlamydia, ureaplasma and mycoplasma, initially affect the urethra in men, causing venereal urethritis. But, like any living microorganism, these infections actively multiply in favorable conditions for them, which are the mucous membranes of the urethra and prostate ducts.
Of course, if the patient consults a urologist or venereologist in time, passes tests for sexually transmitted diseases, discovers the presence of a sexual infection and cures it, then there will be no reason for the appearance of prostatitis. Everything will end with recovery in the stage of anterior urethritis. But in an advanced form of the disease, with a formal approach to the treatment of sexually transmitted diseases, when they are tried to be cured only by taking broad-spectrum antibiotics in tablets, and not cured as a result, microbes penetrate the posterior urethra. and prostate, causing inflammation, i. e. prostatitis, and more often it is primary-chronic at the same time. In this case, it is very easy to avoid the development of prostatitis, absolutely everything depends on the patient himself.
All you need is:
- Seek medical attention immediately at the first sign of urethral discomfort
- Take tests recommended by your urologist for STIs
- Undergo comprehensive treatment for established sexually transmitted infections
- Do control tests after treatment to determine the presence of venereal infection not only in the urethra, but also in prostate secretions
- And it is best to undergo medical prophylaxis in the clinic after casual sex and before the symptoms of sexually transmitted diseases appear and to protect yourself and your loved ones from sexually transmitted diseases in general, and as a cause of prostatitis, in particular
Symptoms of prostatitis
How to recognize or suspect prostatitis in an ordinary person, because its symptoms are very similar to many diseases of the genitourinary system and even other organs? How does prostatitis manifest itself? What are its first signs and how do they behave as the disease progresses. We will talk about it in this article.
What other diseases can be confused with prostatitis:
- Sexually transmitted infections (STIs) are the most common situation when a man comes to a venereologist after a casual relationship, thinking he has an STI. And in fact, the prostate was inflamed.
- Urolithiasis can give similar symptoms, but at the same time it can itself cause an inflammatory process in the prostate.
- Cystitis is rare in men, but the symptoms are very similar to prostatitis.
- Pyelonephritis - inflammation of the renal pelvis has some symptoms in common with inflammation of the prostate.
- Diseases of the scrotum (epididymitis, orchitis, varicocele) - heaviness and pain in the scrotum can accompany these diseases, including prostatitis.
- Diabetes mellitus - patients notice increased urination, as in prostate disease, but there is no slow flow and the volume of urine is normal or even increased.
- Other diseases of the prostate: cancer and adenoma (benign hyperplasia) of the prostate.
- Urethritis.
- Diseases of the rectum - fissures, hemorrhoids, tumors.
- Diseases of the lumbosacral spine.
In order to make a correct diagnosis, a urologist should not only know the symptoms of prostatitis well, but also be able to correctly prescribe tests and other diagnostic studies, as well as be able to adequately evaluate their results.
So, consider the signs or symptoms of prostatitis:
Group 1 is pain syndrome. That is, the appearance of pain in the perineum, groin, lower abdomen, scrotum, penis, rectum, sacrum, coccyx, inner thighs. It can be just pain, a feeling of pulling, pressure, or rather sharp, pulsating, strong pains. Sometimes a man simply complains of discomfort in these areas, both during urination and outside of it. Often, the aching pain intensifies when sitting for a long time in a chair or in a car.
In chronic indolent prostatitis, the pain may decrease after intercourse. If the inflammation is very pronounced in the prostate or large calcifications (stones) have formed in the gland, pain during ejaculation is possible.
Symptoms of group 2 - urination disorders. Increased urination occurs, first at night and then during the day. The stream of urine becomes slow, the volume of each portion decreases, the transparency of urine decreases, blood may appear. In severe swelling of the prostate gland or fibrosis of the gland around the urethra, there are pronounced difficulties in emptying the bladder. A man has to exert himself, wait a while to urinate.
Group 3 - violation of sexual function. In the initial stage of prostatitis, there is a certain increase in sexual desire, hyperexcitability and premature ejaculation. Furthermore, due to the decrease in the production of sex hormones, there is a decrease in libido, a drop in erections. A man either cannot have sexual intercourse, or, having started, cannot finish it. But even when ejaculation occurs, the orgasm is dull or hardly felt at all. If the erection or ejaculation is accompanied by pain, then the man himself refuses new contacts, which, due to long-term abstinence, negatively affects his sexual function in the future. And this also leads to the progression of congestive prostatitis. A vicious circle is created.
Group 4 - these are general symptoms. There may be an increase in body temperature, fatigue, weakness, irritability, which are associated both with the presence of an inflammatory process and hormonal imbalance, as well as with failures in sexual life. Some patients experience hyperhidrosis (profuse sweating) of the inguinal region, redness of the glans penis.
In the case of a sufficiently pronounced inflammatory process in the prostate, there may be mucous or purulent discharge from the urethra.
The clinical picture of each patient with prostatitis is individual. Not all groups of symptoms are necessarily present and not all of them can be expressed. In the case of a chronic process in the prostate, an erased clinic and minor symptoms are observed, but this does not make it the least dangerous for a man's health.
Therefore, if you notice any of the above-mentioned manifestations of prostatitis, make an urgent appointment with a urologist. Do not delay contacting the doctor, because even if the discomfort has passed, this does not mean that the inflammatory process has stopped. It just went into a latent phase and will gradually destroy your health and destroy your prostate.
The best option is a preventive examination every six months by a urologist with diagnostic palpation of the prostate, microscopy of its secretions, ultrasound and blood analysis for PSA. Thus, you protect yourself from the negative consequences of not only advanced chronic prostatitis, but also adenoma and prostate cancer.
Treatment of prostatitis
Modern methods of treatment of prostatitis include the following types:
- drug treatment (prescribing antiviral and antifungal drugs);
- maintenance therapy (prescribing immunostimulating drugs, taking nutritional supplements);
- urological massage (prostate massage);
- LOD-therapy (a method that uses low pressure to restore potency);
- a set of special physical exercises for relaxation;
- doctor's recommendations in matters of nutrition, lifestyle, sexual relations.
In treatment, I use the best methods of leading medical centers and my own developments that give excellent results.
Congestive (congestive) prostatitis
Treatment of congestive prostatitis presents certain difficulties, because the causes of this type of prostate inflammation are the lifestyle and sexual activity of this man. Accordingly, only the patient himself, and not the doctor, can directly influence these processes. But even in such a difficult situation, patients can be helped. For the treatment of congestive or congestive prostatitis, a special complex therapy has been developed that allows you to eliminate the effects of blood stagnation in the venous plexus of the prostate and secretion of the prostate in its channels and acini.
Treatment of congestive prostatitis
After a preliminary diagnosis, which includes:
- Prostate secretion analysis for microscopy, STI, culture
- PSA blood test
- General analyzes of urine and blood
- Blood chemistry
- Ultrasound of the prostate, its venous plexus
- kidney ultrasound
A diagnosis of chronic congestive prostatitis is made, a complex of drug treatment and necessary procedures are determined, which include:
- Prostate massage through the rectum is necessary to remove plugs of leukocytes, mucus and congestive inflammatory secretion of the prostate from the duct of the gland. It is a major treatment procedure that also improves blood flow to the prostate, which serves as a factor in combating blood stasis.
The massage is performed by a urologist. Session duration from 30 seconds to 2 minutes. Quantity of 10 per course. The price is 600 rubles.
Even if the patient does not have the opportunity to complete the entire course of treatment for congestive prostatitis, he must attend at least 10 massage sessions. Taking medication alone does not provide the desired effect in the treatment of prostate congestion.
- Vibromassage of the prostate is a very good and effective procedure for the treatment of congestive prostatitis. With the help of a special device that creates vibrations, thermal and magnetic fields, blood supply to the gland is improved, the attachment of leukocyte plugs to the walls of the prostatic ducts is weakened, which facilitates their removal during subsequent finger massage. It is usually done right before the massage session.
- Magnetic laser therapy improves blood flow and trophism of the gland, removes inflammatory products from it, relieves swelling. Many patients already feel its effect in the first days of treatment in the form of a reduction in pain and tension in the prostate area.
This treatment of congestive prostatitis has long been established and has been successfully used for many years, it is constantly updated, including new modern methods and approaches. Chronic congestive prostatitis can and should be treated, achieving long-term remission and significantly improving the quality of life of a modern man.
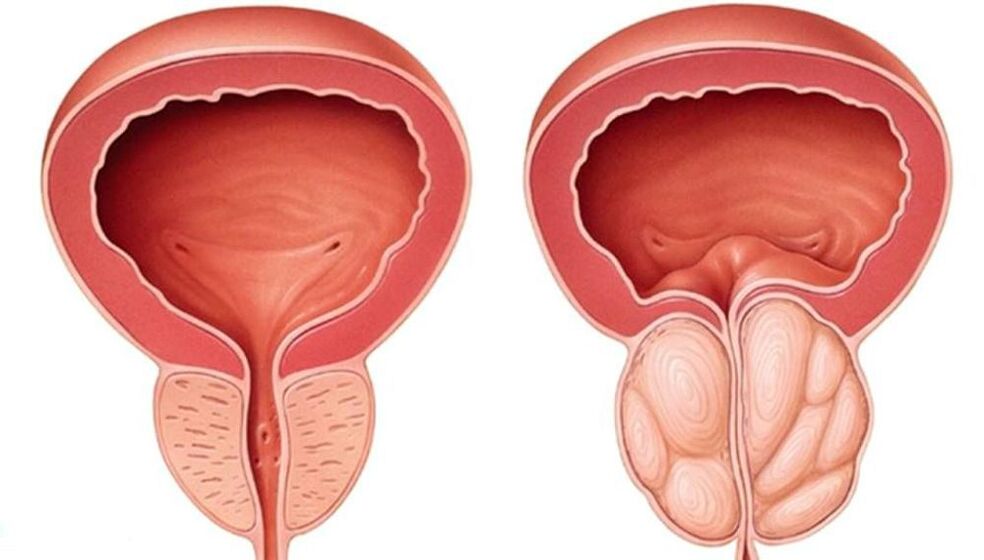
BPH
Prostate adenoma, or as it is commonly called today, benign prostatic hyperplasia (BPH) is a chronic disease that occurs mainly in older men, at least after 50 years. After 70 years, more than 50% of men already have complications of this disease. Although there are cases of its earlier development.
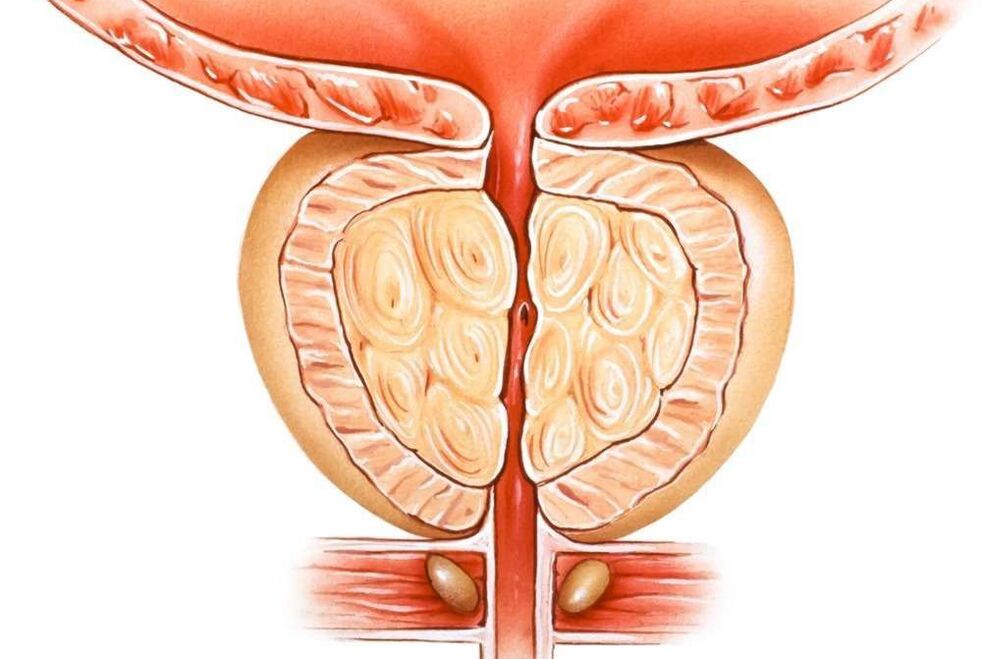
Prostate adenoma is accompanied by the growth of its glandular and stromal (connective) tissue. As a result, knots form in the thickness of the gland, which, when they reach a large size, begin to compress the surrounding tissues - the bladder, urethra, rectum, and sometimes the ureters, disrupting the normal functioning of these organs.
Reasons for the development of prostate adenoma
The development of prostate adenoma is associated with hormonal imbalance in older and older men, i. e. a kind of manifestation of "male menopause". With age, there is a decrease in the production of the main male hormone testosterone in the testicles and an increase in the content of the female hormone estradiol (especially in men with a large body mass). The direct negative effect of female hormones on the prostate has been proven, as well as the increased production of dihydrotestosterone in prostate cells, which causes active growth of its tissue and the development of benign prostate hyperplasia, i. e. adenoma.
Reasons leading to the development and progression of BPH may also include:
- hypodynamia - sedentary lifestyle
- alcohol abuse and smoking
- fatty, spicy, spicy foods high in cholesterol
- low sexual activity
Chronic prostatitis, in principle, is not the cause of prostate adenoma, but with the simultaneous course it contributes to more pronounced symptoms and the rapid development of complications of prostate hyperplasia.
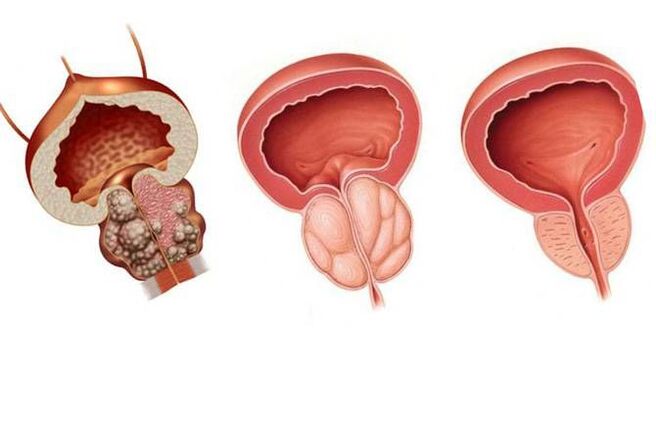
Symptoms of prostate adenoma
Symptoms of prostate adenoma depend on the stage of the disease, its decompensation, the development of complications and the direction of tumor growth.
- First, there are signs of difficulty urinating, slow stream of urine, constant urges up to 15-20 per day, nocturia - nocturnal urination.
- Then, as the muscles of the urinary bladder weaken, pain in the lower part of the stomach is worrying, the feeling of incomplete emptying of the bladder, urine is excreted in portions, drop by drop, it is necessary to strain the abdominal muscles. It ends with the complete loss of the detrusor - the bladder muscles that expel urine.
- In combination with chronic prostatitis, there is pain in the perineum, rectum, elevated temperature, discharge of mucus and pus from the urethra.
- Urine changes color, becomes cloudy, drops of blood may appear.
- Sexual function is impaired.
- With the growth of prostate adenoma towards the triangle of the bladder formed by the mouth of the ureter and the urethra, there is a blockage of the ureter and a violation of the outflow of urine from the kidney, which ends in a faster development of chronic kidney disease. failure and urolithiasis.
Main complications of prostate adenoma:
- Acute urinary retention - requires urgent bladder catheterization.
- Urolithiasis and inflammation of the kidneys (pyelonephritis), bladder (cystitis) and urethra develop as a result of urine stagnation.
- The appearance of blood in the urine.
Chronic kidney failure is a serious complication that can lead to death.
Treatment of prostate adenoma
In the office, prostate adenoma is treated without surgery, that is, drug therapy, which is most effective for 1, and sometimes 2, benign prostatic hyperplasia.
Surgical treatment of prostate adenoma is carried out with decompensation, a large volume of prostate adenoma growth towards the triangle of the bladder. It comes in different types:
- starting with an open transvesical adenomectomy - removal of the tumor through the bladder
- ending with minimally invasive methods, when through the urethra with the help of an electric knife, radio wave and laser techniques, the urethra is freed from adenoma tissue or the hyperplastic areas of the prostate are completely removed.
In order to prevent prostate adenoma surgery being immediately offered to you during your first visit to the urologist, you need an annual prostate examination, an ultrasound and a PSA blood test.
prostate massage
One of the most common and highly effective therapeutic and diagnostic procedures in urology and venereology is prostate massage. This manipulation has long been used by urologists and is known to almost all patients with diseases of the prostate, seminal vesicles and sexually transmitted diseases.
Why is prostate massage used?
Prostate massage can be used in two cases:
for diagnostic purposes for:
- Obtaining prostate secretions for microscopic analysis
- Determination of the presence of sexually transmitted infections (chlamydia, ureaplasma, mycoplasma, gonorrhea, etc. ) in the prostate using PCR, PIF, etc.
- Taking material for culture with determination of microflora and sensitivity to antibiotics
- Obtaining subjective data on pain, density, size of the gland - the so-called. diagnostic palpation of the prostate
for therapeutic purposes:
- to free the ducts of the gland from plugs of leukocytes and mucus
- to improve blood circulation in the prostate, which leads to better penetration of drugs into its tissue and elimination of congestion
When is prostate massage prescribed?
Prostate massage is prescribed for various health problems of men, for example:
- chronic bacterial and abacterial prostatitis
- chronic vesiculitis - prostate and seminal vesicle massage
- chronic and delayed urethritis
- prostatitis caused by genital infections
- erectile dysfunction and infertility associated with prostate diseases
- with a preventive purpose in the treatment of sexually transmitted diseases in the final stage
Prostate massage is not performed in the presence of acute purulent inflammation of the genital organs!
How is prostate massage performed?
There are several classic positions for prostate massage.
The most common position is the knee and elbow position, when the patient is standing on the couch on the knees and arms bent at the elbow joints, bending at the waist.
In the case of spinal diseases, old age, heavy body weight, a position on the left side with legs bent at the knees, brought to the stomach, is possible.
During seminal vesicle massage, the patient stands with his legs on the couch with his back to the doctor and is in a semi-squatting position.
When massaging the prostate, the urologist's index finger is inserted into the patient's rectum and begins to alternately massage the right and left lobes of the prostate, ending with the interlobar groove (isthmus). During this manipulation, which lasts from 30 seconds to 2 minutes, the doctor receives information about the soreness of the gland, its size, consistency, surface, furrow strength and can take the secret of the prostate for analysis.
During the prostate massage, some discomfort, urge to urinate, feeling of pressure in the lower abdomen, penis may occur. With severe pain, the massage stops.
It is very important that this procedure is performed by qualified and experienced urologists or venereologists in order not to harm the man and not to injure the prostate.
Vibromassage of the prostate

Vibromassage of the prostate - the use of vibrations, magnetic field and heating in the treatment of chronic prostatitis. This type of physiotherapy improves blood flow and nutrition to the prostate tissue. Vibromassage helps to remove plugs of leukocytes from the ducts of the gland. In case of calculous prostatitis - one of the alternatives to finger massage. The duration of the session is from 10 to 20 minutes.
Prevention of prostatitis
Prevention of prostatitis consists in avoiding predisposing factors that cause prostatitis, as well as:
- Try not to freeze for a long time, if you spend a long time in a cold room or on the street, take care of appropriate clothing.
- For constipation, use laxatives and don't bother.
- If you have a sedentary job, give yourself a "gym break" every hour (or at least just get up and walk around).
- Try to have a regular sex life, because it is completely in line with a person's normal lifestyle and allows you to avoid many problems, not only prostatitis.
- Try to eat regularly and well, lead an active lifestyle, do not get sick and, finally, just think about your health from time to time.
Also, don't forget to visit your urologist regularly.























